Traumatic injuries to the head and face: Subdural hematoma
This is an excerpt from Acute and Emergency Care in Athletic Training With Web Study Guide by Michelle Cleary,Katie Walsh Flanagan.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
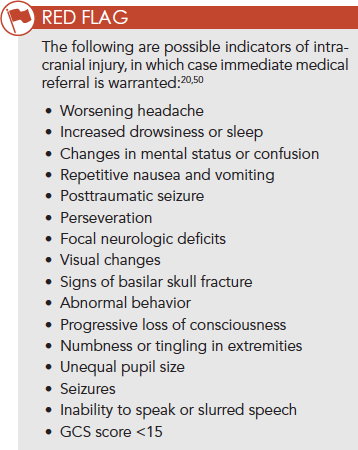
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
More Excerpts From Acute and Emergency Care in Athletic Training With Web Study GuideSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- How do I integrate nutrition education into PE?
- How does the support of friends and family influence physical activity?
- What makes the Physical Best approach unique?
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?


