Relationship between exercise and dementia
This is an excerpt from Advanced Neuromuscular Exercise Physiology-2nd Edition by Phillip Gardiner.
Alzheimer’s disease (AD) is the most common form of dementia. It includes loss of neurons and cognitive decline. Causative mechanisms that have been proposed for the development of AD include free radical damage, inflammatory events, and accumulation of abnormal proteins in the brain. A marker for the presence of AD in autopsy material is the presence of beta-amyloid plaques or neurofibrillary tangles (Brown, Peiffer, and Rainey-Smith 2019; Sujkowski et al. 2022). Studies with rodents have been quite consistent in demonstrating the positive effects of aerobic exercise on these processes, while studies in humans have proven equivocal. In separate studies, exercise has been shown to exert benefits on inflammation and redox status in the brain (Stephen et al. 2017) and on the nervous system, in general, through the exercise-evoked muscle secretion of exerkines and neurotrophins (Severinsen and Pedersen 2020). An active lifestyle may decrease the risk of certain forms of dementia (Aarsland et al. 2010; Santos-Lozano et al. 2016). This leads us to some questions: Do we have hard evidence that exercise positively influences brain structures? Does regular exercise impact memory? Once AD has been diagnosed, is it too late to begin an exercise program?
To examine these issues, I have highlighted three meta-analyses that deal with brain function, aging, and physical activity. Meta-analyses are usually preferable to single studies, even single random controlled trials, because data can be combined to increase statistical power and because the quality of individual studies can be assessed and included or excluded on this basis. Data can also be stratified more effectively, because of sample size, to tease out the effects of age, sex, exercise type, frequency, and duration, among other factors. The first meta-analysis I have highlighted concerns effects of physical activity on episodic memory in seniors that have not been diagnosed with AD. Episodic memory involves recollection of previous life experiences and involves the hippocampus, which shows a neurodegenerative decrease in volume as individuals pass from mild cognitive impairment to AD (Reijs et al. 2017). It is one of the earliest memory systems to decline with advancing age. The second meta-analysis examines the effect of exercise once AD has been diagnosed, while the third addresses the issue of the effects of exercise on hippocampal volume.
Aghjayan and colleagues (2022) conducted a meta-analysis of 36 randomized controlled trials involving a total of 2,750 subjects to determine if aerobic exercise has an effect on episodic memory among individuals within the age group of 55 to 85 yr with normal cognition, subjective cognitive decline, or mild cognitive decline. Outcome measures for episodic memory included a word list, story recall, face or name recognition, object memory, or paired associates. Their analysis confirmed that aerobic exercise improves episodic memory. They also found that it was the people with normal cognition and those who were younger who benefited, not those with cognitive impairment. Benefit was seen when the exercise program was 15 to 90 min, three sessions per week, for 18 to 39 wk, to achieve greater than 3,900 total minutes of activity.
López-Ortiz and colleagues (2021) conducted a systematic review and meta-analysis of exercise interventions for AD. They meta-analyzed 21 randomized controlled trials on Alzheimer’s patients published since the year 2000. The patients in their eighth and ninth decades had been diagnosed with AD. Exercise programs ranged from 1 to 7 d/wk, were supervised, and lasted between 9 wk and 12 mo. The outcomes measured included cognitive function, physical function (6 min walking test), an index of functional independence, and neuropsychiatric symptoms. Most studies involved a combination of aerobic (mild to moderate intensity) and resistance exercise. Some used aerobic exercise (mild to moderate intensity) only, and some used resistance exercise only. The authors indicated that considerable heterogeneity was found for most results and concluded that exercise interventions might improve some markers of functional independence, physical function, balance, and neuropsychiatric symptoms. Interestingly, the benefit for exercise interventions to improve cognitive function was merely a trend, with actual significance reached when the aerobic exercise–only group was analyzed separately.
The last meta-analysis here concerns the effect of exercise on the volume of the hippocampus itself. Wilckens and colleagues (2021) analyzed 22 randomized controlled trials with 1,204 participants published since 2010 that included an exercise intervention (14-39 wk) and that had made before and after measurements of hippocampal volume. Subjects included healthy controls and patient groups with various characteristics: documented tendencies toward reduced hippocampal volume, mild cognitive impairment or early AD, depression, obesity or type 2 diabetes, schizophrenia or psychosis, and radiation-treated children. The result of the analysis was a significant positive effect from aerobic exercise on hippocampal volume. Most of the significant effect was due to a loss of hippocampal volume in the control group, suggesting that exercise can attenuate age- and disease-related loss of hippocampal volume. The effect was most significant for the older subjects and for interventions lasting greater than 24 wk.
The takeaway here seems to be that exercise has a positive effect on episodic memory and hippocampal volume (figure 11.3), and for AD patients, quality of life, physical function, and neuropsychiatric symptoms. These analyses also seem to suggest that exercise started too late in the dementia disease process may be less effective than before the symptoms appear.
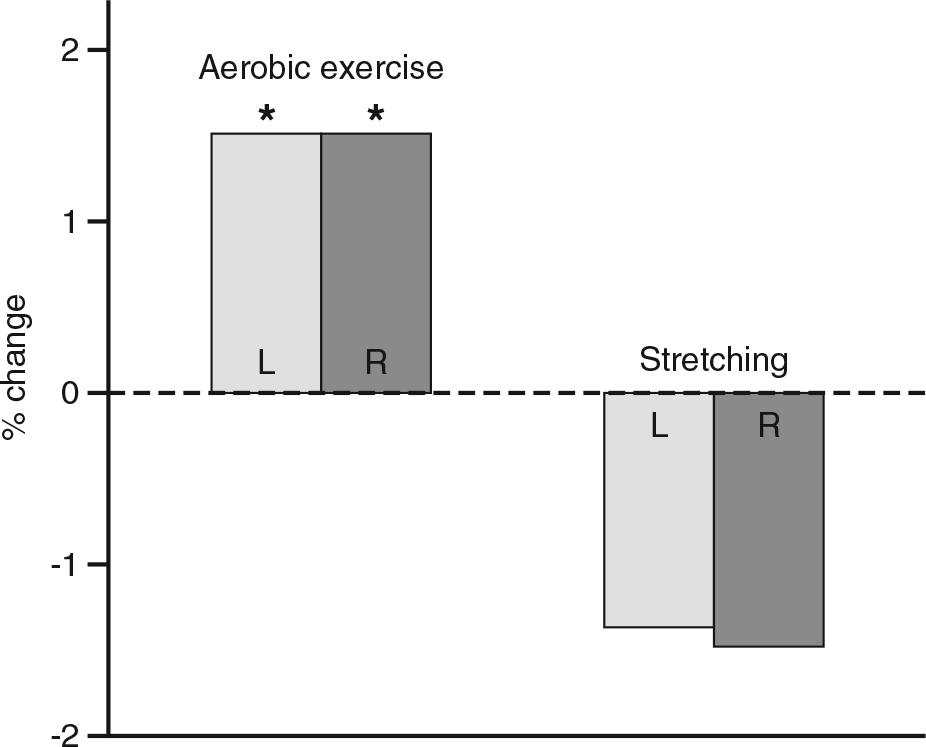
Data from Wilckens et al. (2021).
Key Point
A lifestyle including regular physical activity appears to reduce the risk of developing dementia. In the near-elderly, if exercise is initiated before cognitive decline is evident, episodic memory can be improved. Once dementia is diagnosed, exercise can improve functional independence, physical function, balance, and neuropsychiatric symptoms, but cognitive improvement requires an important aerobic exercise component be included in the exercise program. Regular exercise also reduces the age-associated loss of volume of the hippocampus, the principal site of memory consolidation.
More Excerpts From Advanced Neuromuscular Exercise Physiology-2nd EditionSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW


