Postural tests for formal assessment
This is an excerpt from Low Back Disorders 3rd Edition With HKPropel Access by Stuart McGill.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
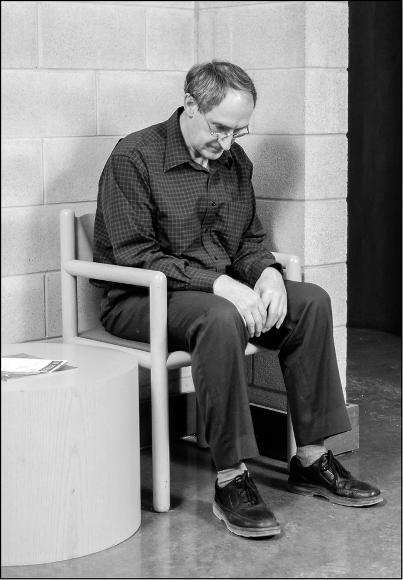
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |
 |
 |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |
 |
 |
|
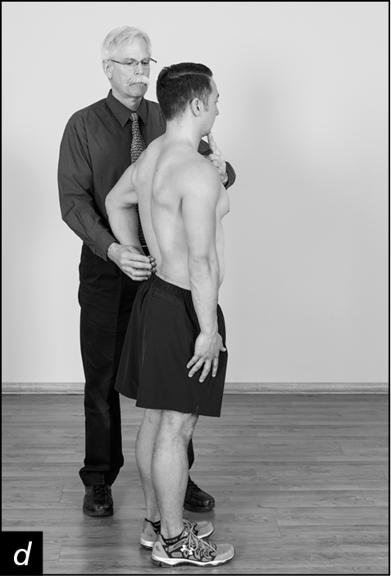
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |
 |
 |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
More Excerpts From Low Back Disorders 3rd Edition With HKPropel AccessSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW