Heat-related emergencies in athletes
This is an excerpt from Acute and Emergency Care in Athletic Training With Web Study Guide by Michelle Cleary,Katie Walsh Flanagan.
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
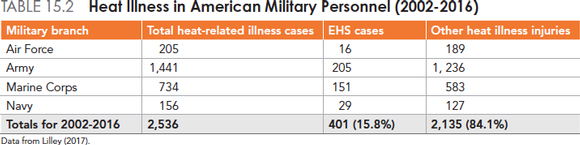
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
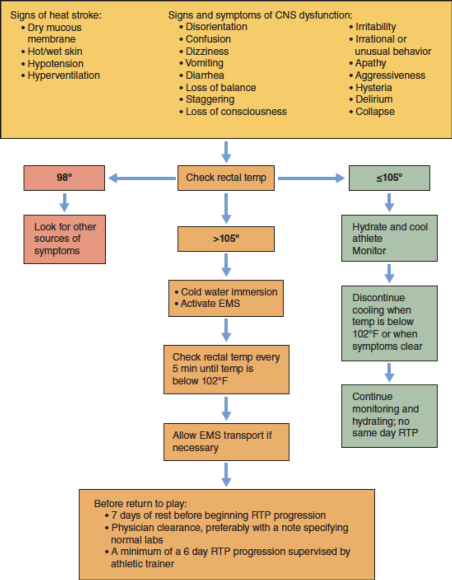
Figure 15.1 Decision tree for EHS.
More Excerpts From Acute and Emergency Care in Athletic Training With Web Study GuideSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- How do I integrate nutrition education into PE?
- How does the support of friends and family influence physical activity?
- What makes the Physical Best approach unique?
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?