Considerations for the prescription of exercise and physical activity
This is an excerpt from Guidelines for Cardiac Rehabilitation Programs 6th Edition With Web Resource by .
By Jonathan Myers
Guideline 6.1 Considerations for the Prescription of Exercise and Physical Activity
When developing an exercise prescription, consider the following factors:
Safety Factors
- Clinical history
- Risks associated with CVD progression or instability
- Ischemic and angina thresholds
- Cognitive or psychological impairment
Associated Factors
- Vocational or avocational requirements
- Orthopedic limitations
- Previous and current activities
- Personal health and fitness goals
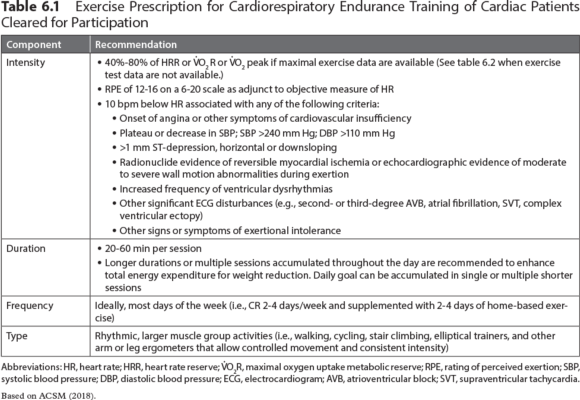
An important initial consideration in exercise planning is safety. Safety considerations apply to both structured exercise training and leisure-time PA. While most patients can engage in exercise without incurring undue risks, appropriate risk stratification should be performed. Guideline 6.1 provides key variables to consider when developing an exercise prescription. Safety and risk stratification are discussed in detail in chapters 4 and 5. Recommendations for supervision and ECG monitoring can be found in chapter 5. Later in this chapter, tables 6.1 and 6.2 present basic principles of exercise prescription. A model for risk stratification for cardiovascular events is outlined in the sidebar Stratification of Risk for Cardiac Events During Exercise Participation in chapter 5. After risk stratification, recommendations for supervision, ECG, monitoring and prescribed intensity and duration of exercise training can be made.
Comprehensive, evidence-based recommendations for structured exercise training in CR are available from several prominent organizations1,3,8 and are only summarized here. A comprehensive exercise program includes cardiorespiratory, musculoskeletal, and flexibility components. Specific elements for each component are summarized in the tables in this chapter and include guidelines for intensity, duration, frequency, and type of exercise for training. Each of the elements should be prescribed relative to one another and in a way that effectively addresses predefined training goals (e.g., increased aerobic or musculoskeletal fitness, weight reduction, control of blood glucose, or resumption of occupation).
Cardiorespiratory Endurance Training
Cardiorespiratory endurance training should be the foundation of most exercise routines for adults with or at risk for CVD. This type of exercise training is the most effective way to increase CRF. Elements of an exercise prescription for increasing CRF are presented in table 6.1. The relative training intensity may vary between 40% and 80% of maximal heart rate reserve (HRR) or metabolic reserve (V.O2R). Initially, programs should focus on the lower part of the intensity range, with progression to higher intensities as patients adapt to the program.7 RPE (e.g., Borg Scale of Perceived Exertion 6-20; Borg CR10 Scale; Omni Picture System of Perceived Exertion) are considered adjunctive to HR monitoring, but they may become more important as a subjective intensity guide as patients gain experience with exercise training and learn how to use the scale. Exercise training duration varies as a function of the overall energy expenditure goals of the patient. A minimum of 20 continuous minutes of exercise per session is commonly recommended within structured programs, although some patients may follow an intermittent (i.e., interval) exercise regimen. Some patients may need to accumulate shorter bouts (e.g., multiple 10 min bouts) throughout the day due to comorbidities, symptoms such as claudication or musculoskeletal discomfort, or lifestyle factors. Ideally, patients should be active most days of the week,1-7,9 but structured programs are often designed with a frequency of two to four sessions per week.
Once the initial exercise prescription is established, patients should progress gradually toward predefined or redefined program goals. There is no set format with respect to progression because many factors, including fitness level, motivation, and orthopedic limitations, influence the rate at which a patient may progress. In general, it is prudent to change one component and provide some time (a minimum of one exercise session) to assess the adaptation to the new level before progressing further. When time permits, increases in duration and frequency should precede increases in intensity. Modest increases in intensity, when appropriate, are likely to be tolerated and should be based on the observations of the staff and subjective responses of the patient, provided that the changes remain within the limits specified in the most recent evaluation.
A guiding principle should be progression of the total volume or dose of exercise such that the patient achieves desired energy expenditure thresholds within a three- to six-month period. Therefore, given that most patients' participation in CR lasts no longer than three months, it is important to educate and encourage patients to continue exercising even after CR participation has ended. The most appropriate volume of exercise depends on the individual CVD risk profile, training goals, and comorbidities (i.e., diabetes, hypertension, obesity, arthritis). An accumulating body of evidence has affirmed a dose-response relationship between the volume of PA and health outcomes.1,3,6-8 Whether exercise has a role in reversing coronary artery disease is an issue that remains controversial; however, thresholds of approximately 1,500 and 2,200 kcal/week are associated with stability and regression of coronary artery lesions, respectively.18 Notably, multiple studies document that energy expenditure in structured CR does not typically meet either of these thresholds.11-14 Therefore, patients will likely need to engage in PA outside of the structured program to achieve the optimal levels of energy expenditure.
Few studies have supported the efficacy of structured exercise training as a singular strategy to normalize body weight and body composition in patients with CVD. This underscores the importance of multiple behavioral strategies in weight reduction programming for overweight patients. Studies show that achieving weight loss goals requires a simultaneous change in dietary habits in addition to greater physical activity patterns. The volume or dose of exercise associated with the typical CR training session may be a limiting factor, and there is only a 1 to 2 kg weight loss during CR participation. It is likely part of the explanation for a low amount of weight loss during CR is due to a lack of focus on helping patients lose weight. As mentioned previously, numerous studies have shown the weekly dose to be inadequate for weight or fat reduction. As an example, a typical exercise session for an outpatient with a peak functional capacity of 7 METs might be 30 min at a heart rate that would equate with about 4 METs. The following formula provides a method to estimate the caloric costs of the exercise session:
Calories/min = [METs × body weight in kg × 3.5] / 200
It should be noted that the 4 MET value in this example includes the resting energy expenditure component (1 MET). Therefore, the net caloric cost of the exercise would be based on only 3 METs. If the hypothetical patient in this example weighed 100 kg (220 lb) and exercised 3 days per week for 30 min, the net caloric expenditure would be approximately 480 kcal/week (5.3 kcal/min × 30 min × 3 days/week). Although patients can clearly improve exercise tolerance with this regimen, the estimated caloric expenditure falls well short of contemporary recommendations for PA and in most cases would not be effective for weight or fat loss.15 For example, 40 min sessions, five times per week, would result in an expenditure of approximately 1,060 kcal per week. Again, this calculation highlights the importance of increasing PA outside of the structured or in-hospital program. Thus, adjustments must be made about frequency and duration of exercise to allow patients to achieve greater energy expenditures to enhance program outcomes. However, these adjustments must be with the caveat that although it is prudent to increase exercise volume progressively, staff must carefully consider the risk that a higher-volume program may lead to higher dropout rates. Therefore, overweight patients must be educated about the need to develop and maintain fitness as the core of their exercise regimen, with the additional volume of PA facilitating weight loss and other goals. Finally, as CRF improves, patients are able to exercise at a higher metabolic rate (more kcal/min) at a given relative intensity (% maximal HRR). This adjustment allows patients to accumulate a greater caloric deficit over time.
More Excerpts From Guidelines for Cardiac Rehabilitation Programs 6th Edition With Web ResourceSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- Women in sport and sport marketing
- Sport’s role in the climate crisis
- What international competencies do sport managers need?
- Using artificial intelligence in athletic training
- Using the evidence pyramid to assess athletic training research
- How can athletic trainers ask a clinically relevant question using PICO?


